Quality Control Monitoring for Euploid Embryo Transfers
Our clinic and lab have made several changes to improve outcomes of euploid embryo transfers over the past several years.
First, we have switched most of our PGT-A testing to high density SNP (Single Nucleotide Polymorphism) testing rather than NGS (Next Generation Sequencing). Specifically we use the LifeView SNP testing platform by Genomic Prediction. Genomic Prediction had claimed that their testing is more accurate than NGS resulting in both higher euploid call rates and higher pregnancy rates. We have been able to replicate these findings with our own data. It seems that the high density SNP testing by LifeView results in 5-10% more euploid embryos and 5-10% higher ongoing pregnancy rates than testing with other platforms. There are no formal publications on this and the data is difficult to obtain with certainty due to the high numbers needed to detect these small differences with confidence.
Second, in 2025 our lab switched biopsy techniques from assisted hatching on day 3 for biopsy on days 5, 6, and 7 to hatching and biopsy concurrently on day 5, 6, and 7.
Lastly we have switched more of our FET (Frozen Embryo Transfer) protocols from hormone replacement cycles (estrogen for about 2 weeks followed by the addition of progesterone and transfer on the 6th day of progesterone) to modified natural cycles without letrozole (Femara). Typically a natural FET cycle consists of no medications and just ultrasound and bloodwork monitoring with embryo transfer about 5 days after ovulation (about 6 days after the LH surge). Most of the time the term “modified” is used to indicate that an HCG trigger is given to trigger ovulation. Technically a modified natural cycle has a much more broad definition encompassing all FET cycles where an ovulation occurs and any additional medication is used. This could be medication to stimulate ovulation (such as letrozole, clomid, tamoxifen, FSH, Menopur, or others), trigger ovulation (typically HCG subcutaneously), and/or luteal phase support (typically vaginal or IM progesterone).
We use the term “modified natural cycle without letrozole” somewhat loosely to indicate what we consider an optimal modified natural cycle. This includes the following criteria:
No use of letrozole, clomid, or tamoxifen.
Ok to use gonadotropins such as Follicle Stimulating Hormone or Menopur (typically these are used for anovulatory patients with PCOS). We like FSH 75 units subcutaneously (SC) every other day starting on menstrual cycle day 3. Some patients require FSH 75 units SC daily.
Can be with or without HCG trigger. Sometimes patients ovulate naturally and embryo transfer timing can be based off of US and bloodwork data taken before and after ovulation. Sometimes when a patient ovulates naturally we still have them take the HCG trigger.
Ok for euploid embryo transfer after a fresh oocyte retrieval. We have data on about 5 of these and pregnancy rates look good.
Ok with or without luteal phase support. Ok for luteal phase support with any kind of progesterone (vaginal or IM are most common).
We also consider total natural FETs to be an optimal transfer though not technically a modified natural FET. We have seen a fetal hearbeat from 3 out of 5 euploid embryos transferred in total natural FETs (no ovarian stimulation, no trigger injection, no luteal phase support, no medications of any kind related to fertility).
Our most common modified natural FET protocol is ultrasound on cycle day 10-12 (we prefer day 12), one Ovidrel trigger (subcutaneous HCG) when the lead follicle is expected to be about 17-23mm in mean diameter, and vaginal Prometrium 200mg daily starting 4 days after HCG trigger. We perform the embryo transfer 7 days after the HCG trigger. For example if the HCG trigger is on Monday June 1st the transfer would be on Monday June 8th. Wednesday June 3rd would be considered the first day of progesterone exposure for the endometrium so that June 8th would be the 6th day of progesterone exposure.
We try not to see patients more than 1 time for US and bloodwork monitoring unless the lead follicle is < 14mm at the monitoring US. We typically don’t change the transfer date if the LH is elevated on the day of trigger but sometimes do consider moving the transfer up a day for LH surge (particularly if this prevents embryo transfer on a Sunday since we try to minimize lab procedures on Sunday). Moving the transfer date based on LH surge is considered on a case by case basis.
Our rate of utilization of “modified natural FET without letrozole” protocols for euploid embryo transfers increased from 4% in 2023 to 17% in 2024 to 45% in 2025 (this is through the present date of 5/25/25 which consists of transfers through 4/25/25). In 2024 we started to see a trend that modified natural cycles were better only when letrozole was not used and this became more certain through the later part of 2024 and early 2025.
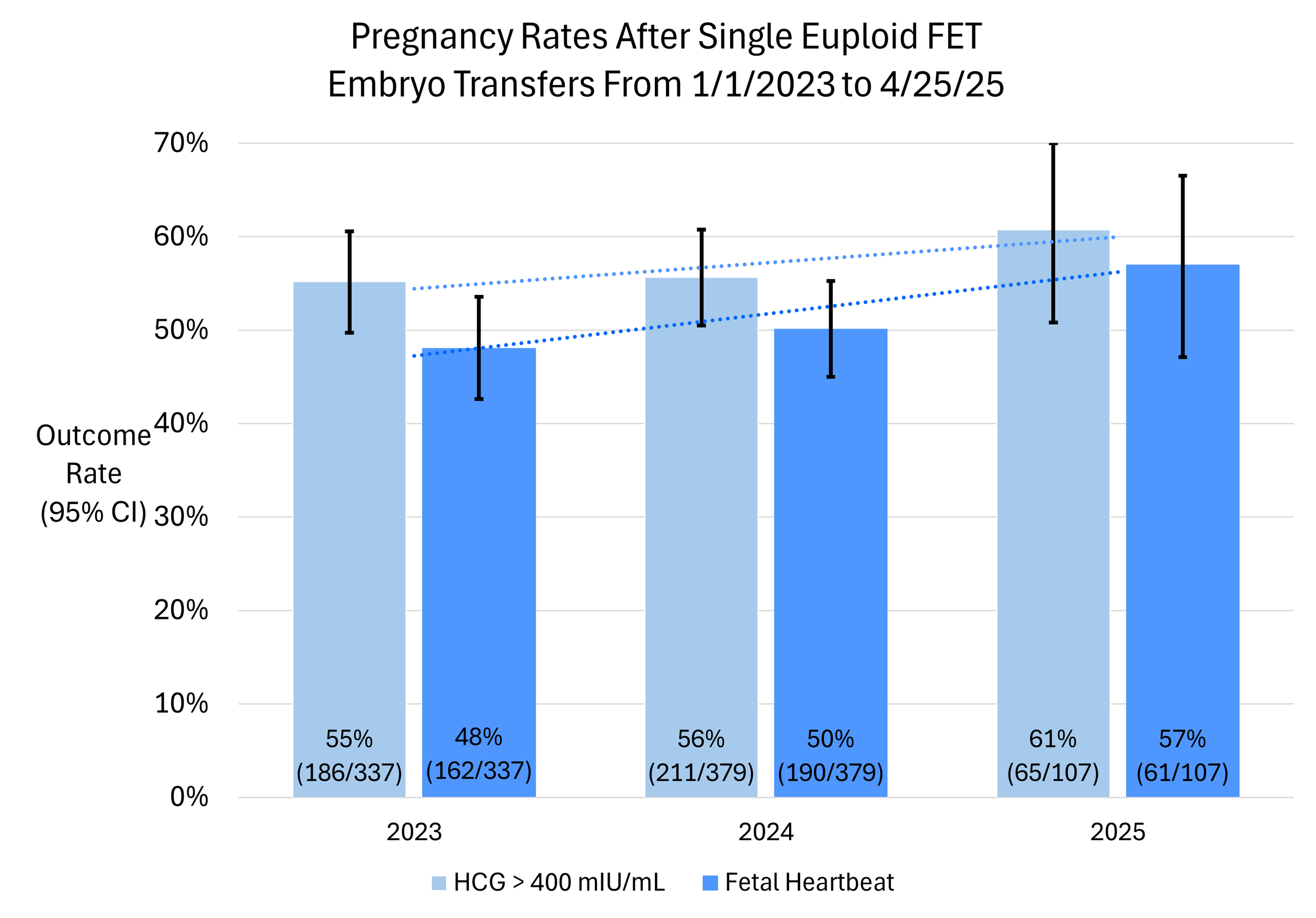
The following graph shows how our outcomes data improved in the past two and a half years. We attribute this mostly to the shift in use of modified natural FET protocols without letrozole and also to a lesser extent the slow but steady improvement in the biopsy technique of our embryologists.
What is notable here is not only the increase in rate of positive HCG above 400 mIU/mL (measured 14 days after embryo transfer at 4 weeks 5 days gestation) and fetal heartbeat but also that the gap between the two narrows. What we seem to be seeing is that there is less drop off from + HCG to seeing a fetal heartbeat when a corpus luteal is present. The corpus luteum is the life support for the embryo and makes many hormones and proteins other than just estrogen and progesterone. With the corpus luteum present missed doses of progesterone are not catastrophic for the pregnancy. With modified natural FET without letrozole we are seeing a fetal heartbeat rate of 67% per euploid embryo (2023 through present). This would correspond to about a 62% live birth rate (67% x 0.93 = 62%). We generally see that when there is a fetal heartbeat a live birth will results about 93% of the time and we use this as a rule of thumb.
In the SART 2023 database there were 38,420 single PGT-A tested embryo transfers for women < 35 years old which resulted in a 53% live birth rate per single PGT-A tested embryo.
It seems that the upper limit of possibility is a live birth rate of 60-70% for a single euploid embryo.